
"Early diagnosis and intervention will help to alleviate you or your child’s symptoms, therefore improving quality of life."
"Early diagnosis and intervention will help to alleviate you or your child’s symptoms, therefore improving quality of life."
Eczema, also referred to dermatitis, is a chronic inflammatory skin disorder which presents in both children and adults. It usually results in dry, inflamed and scaling skin that feels chronically itchy. Depending on the type of eczema, patients may experience symptoms at varying severities.
The National Skin Center reports that at least one in every ten adults in Singapore suffers from eczema. What is even more worrying is the fact that the number of people diagnosed with this condition keeps increasing with at least eight new cases reported every day.
There are two main types of eczema; contact dermatitis that is caused by direct skin contact with external triggers and endogenous dermatitis that occurs as a result of conditions within the body, a common example is atopic dermatitis.
Contact dermatitis refers to a red and itchy rash caused by an allergic reaction or direct skin contact with an irritant.
Allergy contact dermatitis occurs when your skin develops an allergic reaction when exposed to foreign substances. This exposure causes your body to release different inflammatory chemicals that make your skin irritated. The common causes of allergy contact dermatitis include perfumes or chemicals in skin care products or cosmetics, jewelry made from gold or nickel, and latex gloves.
Irritant contact dermatitis is the most common type of contact eczema. It occurs when your skin comes into contact with any toxic material such as bleach, battery acid, detergents, pepper spray, or kerosene. It may also happen when your body comes into contact with less toxic substances such as soap or even water.
Atopic dermatitis is a type of skin inflammation that causes red, scaly, dry and excoriated skin. Atopic dermatitis commonly starts in infancy after the age of 2 months old but some patients may present in later in childhood or adulthood. Most children diagnosed with atopic dermatitis improve as they get older. However, the condition can recur even after an inactive period.
Atopic dermatitis commonly affects the face and scalp in infants, and the flexural areas (eg. neck, elbows and behind the knees) in children. In severe cases, it can become generalised and may affect quality of life. In long-standing cases, the skin can become quite thick due to constant rubbing and scratching of the skin.
One in five children in Singapore suffers from eczema, out of which up to 60% develop this skin condition within their first year of life. The term “atopic” is used to describe an inherited tendency of being hypersensitive to a wide range of environmental factors. Kids diagnosed with atopic dermatitis usually also suffer from other atopic conditions such as allergic rhinitis and asthma.
Medical researchers acknowledge the fact that there is no proven cause of eczema. However, most of them believe that a combination of genes and an external or internal trigger can lead to eczema.
Research shows that most of the patients who suffer from this condition tend to have an over-reactive immune system that produces the inflammation when triggered by either internal environment or external substances. It is this inflammation that causes the itchy and sometimes painful symptoms of eczema.
Research has also revealed that some patients with dermatitis have a gene mutation responsible for creating filaggrin – a special protein which primary role is to help your body maintain a healthy and protective barrier on the top layer of your skin.
If your body fails to produce enough filaggrin to build the protective layer, you end up losing a lot of moisture, letting in bacteria and other viruses ultimately leading to chronic inflammation. This is the primary reason why many individuals with dermatitis have dry and infection-prone skin.
However, we advise not to avoid your child’s vaccinations but to moisturise the skin regularly during the period.
The role of food allergy in triggering atopic dermatitis is controversial. Food allergy is more commonly seen in young children instead of adolescents or adults. If there is suspicion of a food allergy, further testing using skin prick test or blood test can be offered.
Typically, no lab tests are needed to identify eczema. Your dermatologist will perform the diagnosis by reviewing your medical history and examining your skin. He/she may also use the following tests to determine the conditions that accompany dermatitis or rule out other skin diseases:
This will require a small sample of your blood to look for high levels of eosinophils cells in your blood that are part of an immune reaction. Furthermore, a blood test may be performed to check for high levels of a molecule referred to as IgE antibody. An analysis of these blood components will help detect common food and environmental allergies.
In patch testing, small patches that are covered with allergens are usually placed on the patient’s skin for approximately 48hours then removed and the skin reaction evaluated for atopic eczema. Patch testing can be used to identify contact allergies to various products such as metals, fragrances, rubber, etc.
In a skin prick test, a diluted allergen is applied to your skin using a small and disposable plastic device. The skin is then observed for about 20 minutes to see how it reacts. If the surrounding area becomes red and itchy, it indicates the presence of allergy. It is advisable to avoid anti-histamines a week prior to the test.
During a skin biopsy, a doctor numbs the skin and then removes a small skin sample that is used to rule out other skin diseases that can mimic eczema.
Atopic dermatitis can be chronic and persistent. Early diagnosis and intervention will help to alleviate your or your child’s symptoms and therefore improve quality of life. You can start by consulting a dermatologist who is experienced and knowledgeable in eczema.
Topical management with different formula of moisturizer, steroid cream and non-steroidal cream containing tacrolimus, as well as with antihistamines if necessary are the mainstay treatment plan. Wet wrapping is another effective treatment method for severe dermatitis. It involves wrapping the affected area with wet bandages for rehydration and soothing purposes. Counselling on the topical management by a dermatologist or dermatology trained nurses will guide you on management of eczema flare.
Sometimes, your doctor may recommend in-patient treatment if your condition is severe. Under the in-patient treatment options, the doctor may use several methods to manage your situation. This may include a combination of counselling, therapy, and wet treatment. Once your condition stabilizes, you will be allowed to go back home.
In more severe and persistent eczema despite appropriate topical treatment, your dermatologist will discuss the other alternatives such as phototherapy, oral immunosuppressants and the latest biologic injection treatment such as dupilumab.
— Reduce the level of house dust mites. Avoid stuffed toys, pets and carpets in the home.
— Avoid strong soaps and bubble baths.
— Take a short (10 min) bath or shower daily with tepid or slightly warm water.
— A soap substitute is recommended. Sometimes, an antiseptic wash may be prescribed for patients with frequent skin infections.
— Avoid extreme temperatures and excessive sweating if possible e.g. stop physical activities during an acute flare up.
— Minimise scratching. Cut and file fingernails regularly.
— Moisturise two to three times daily with a fragrance-free moisturiser. Apply the moisturiser liberally
— Topical steroids are used as the main treatment during an acute flare of AD.
— The strength of the steroids will depend on the age of your child, as well as the location and severity of the eczema.
— They should be applied twice daily depending on the instruction of your child’s doctor.
— Topical steroids are to be applied on the red, itchy and bumpy areas. Stop application once redness and itchiness resolves and skin is flat.
— Prolonged use of potent or super potent topical steroids can lead to side effects like skin thinning, easy bruising, stretch marks (striae) and increased hair growth. However appropriate use under doctor’s supervision will help to alleviate the itch and improve quality of life.
— These are non-steroidal creams used to treat AD, with a better side effect profile compared to topical steroids. It may not be suitable during an acute flare up.
— Wet-wrap therapy involves wearing wet soft cotton netting above a layer of topical steroid (commonly mild steroid cream) and thick layer of moisturiser. The reason for this therapy is to encourage absorption of topical treatment into the skin and avoid the patient from scratching. Our nurse and doctor will demonstrate the usage of wet wrap.
— These may be prescribed to relieve itch and help you/your child sleep better at night, but not recommended for long term use.
— If there are any signs of skin infection, e.g. pain and weepy rash, oral antibiotics may be warranted.
— In severe cases, oral steroid may need to be prescribed to hasten recovery. If the flare ups are frequent, an oral immunosuppressant may be required to control your skin or your child’s skin conditions.
No. Although atopic eczema can be inherited, it is neither contagious nor infectious and cannot be transmitted from person to person.
The common symptoms of eczema include skin itching, a burning sensation, cuts, skin rashes, red bumps that may ooze or weep, inflammation, and dry, red skin.
If your child shows the symptoms mentioned above, then there is a high probability that he/she is suffering from atopic eczema. It will be most appropriate to bring him or her to an accredited Dermatologist for diagnosis and possible treatment plans. According to the Dermatology Society of Singapore, atopic eczema is common among families with a history of dermatitis.
In most cases, the child will outgrow atopic eczema. Research shows that eczema is rampant among children below the age of five years. However, more than half of these cases usually clear up with age, and only a few will persist into adulthood.
Food allergies have been linked to atopic eczema in only ten to fifteen percent of the reported cases in Singapore. The most common sensitivities are milk, wheat, eggs, fish, and nuts. If you suspect that your child suffers from a food allergy, be sure to visit a dermatologist who will assess your child’s condition and provide helpful recommendations concerning the child’s diet.
We have natural steroid in our body. Steroids work by decreasing inflammation and reducing the activity of the immune system. Topical steroids applied to the inflamed skin will help to control the symptoms of itch and reduce the redness locally.
If topical steroid is used in its appropriate strength, quantity, duration and at the correct sites under your doctor’s supervision, skin damage is extremely uncommon. Without using topical steroids, the skin becomes thick, itchy and unsightly. Delayed use of topical steroids leads to worsening of eczema and stronger topical steroids will eventually be required for longer periods of time.
The skin is often broken and cracked due to inflammation and scratching. Topical steroids help to reduce the inflammation and speed up the healing process. If your skin is very weepy, it may be infected, so antibiotics may be required.
Topical steroids are almost never absorbed into the bloodstream, and so will not affect growth and development or cause other side effects within the body. Short courses of oral steroids may be prescribed for severe eczema flare-ups, but this will not harm the body in the long run. However, repeated courses of oral steroid is not recommended. Untreated severe eczema can have a significant impact on sleep, mood, and daily activities, e.g. school or work. Consequently it will impact on physical, psychological and social development, and this can affect growth and development.
There is no evidence that topical steroids cause dependence or addiction. The reason behind the frequent flare of AD and the need to use topical steroid repeatedly is because the previous flare was not treated adequately and therefore the existing inflamed skin flares soon after the topical steroid was stopped.
In mild cases, moisturiser can sometimes have a steroid sparing effect. Moisturiser should be used daily to relieve dryness of the skin and the frequency of use needs to be increased during a flare. Inflammed and itchy skin requires topical steroids for effective treatment.
Under-treating the affected skin with topical steroid will result in prolonged application and delayed healing of the skin. A useful way of knowing the correct amount of topical steroids to apply is to use the fingertip rule.
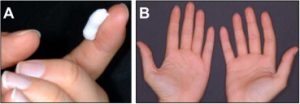
(A) 1 finger tip unit of topical steroid should be sufficient to treat (B) an area of inflamed skin equivalent to two palm surfaces.
| Potency | Name |
|---|---|
| Very mild | Hydrocortisone 1% |
| Desonide 0.5% | |
| Mild | Betamethasone 0.025% |
| Moderate | Betamethasone 0.05% |
| Strong | Betamethasone 0.1% |
| Fucicort (contains antibiotics) | |
| Momethasone furoate | |
| Hydrocortisone aceponate | |
| Very Strong | Clobetasol |
| Fobancort (contains antibiotics) |
Eczema is a common recurrent itchy skin disorder that affects both children and adults. Though currently there is no cure for eczema, it can be adequately controlled to improve quality of life. The primary goal of treatment is to prevent skin inflammation, infection by using appropriate dermatologist-recommended moisturiser. Seek help early from a qualified dermatologist if your itchy skin condition does not improve with simple moisturization.
Gleneagles Medical Centre
6 Napier Road, #06-01
Singapore 258499
Clinic Hours:
Monday, Tuesday, Thursday & Friday
8am to 1pm
2pm to 5pm
Wednesday and Saturday
8am to 12pm
Contact Information
T: +65 6254 6646
F: +65 6259 9853